DISCOVER
AFHTO TEAMS
Formed in 2006, the Association of Family Health Teams of Ontario is a network, resource hub, and advocate for team-based primary care across the province.
DISCOVER
AFHTO TEAMS
Formed in 2006, the Association of Family Health Teams of Ontario is a network, resource hub, and advocate for team-based primary care across the province.
Your Partner on Primary Care
(+ 400,00 unattached served)
Make up our membership – which includes 2700+ family physicians, 450 nurse practitioners, 500+ nurses, and 1300+ interprofessional healthcare providers.
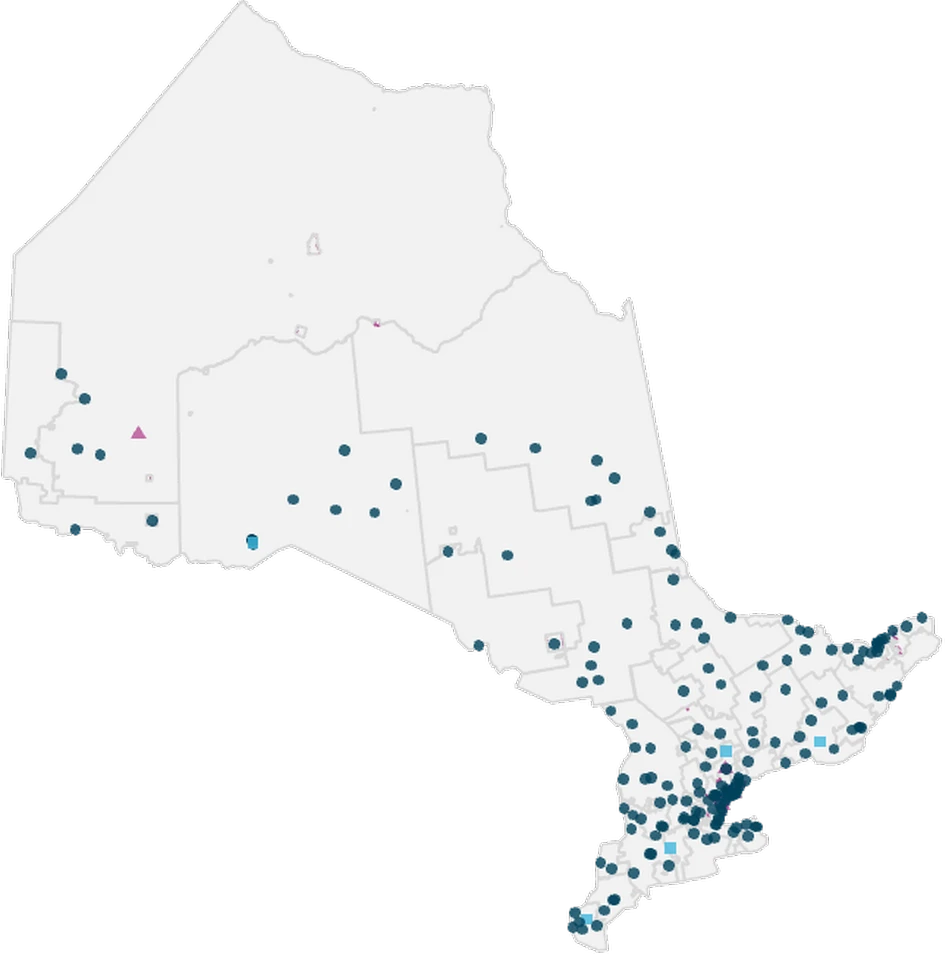
Our province-wide footprint enables us to deploy solutions rapidly and communicate real-time local conditions
THE TEAM-BASE
MODEL
Was announced in 2025 to support primary care expansion – AFHTO’s longstanding advocacy efforts in collaboration with many other professional associations and partners have led to this historic investment.
Current Team Statistics
25%
While 25% of Ontarians are attached to Family Health Teams (FHTs), only 16% of Ontarian family physicians work in FHTs, reflecting the outsized role FHTs play in driving attachment.
1
Community Health Centres
181
Family Health Teams
1
Indigenous Primary Health Care Organization
5
Nurse Practitioner-Led Clinics
2
Other Models of Primary Care
AFHTO MEMBERS BY GOVERNANCE MODEL
Wrong shortcode initialized
AFHTO has a 98.9% retention rate – this means that 98.9% of primary care teams have maintained their membership with AFHTO from 2024-2025 to 2025-2026.
TEAMS ARE HERE.
They’re working.
They’re scalable.
And the system already depends on them.
Find a Primary Care Team
Patients and system partners looking to connect with a team can use AFHTO’s interactive team finder — a searchable directory of primary care teams across Ontario, including FHTs, CHCs, NPLCs, and AHACs.
For those without a family doctor or nurse practitioner, the provincial Health Care Connect program can help link people to a primary care provider and team in their community.

Emerging Leaders Across Primary Care Teams
Check out AFHTO members who are rising stars in primary care, actively shaping the future of team-based care. Emerging leaders are early- to mid-career professionals (5–10 years) from either clinical or operational backgrounds who demonstrate initiative, innovation, and collaborative leadership. These individuals are driving meaningful change and already show the promise of future system leadership. They lead not by title, but through action, vision, and the ability to bring others along.

Elizabeth Smith
Advancing nurse practitioner leadership
- Data-driven leadership
- NP advocacy
- Strong mentor
Elizabeth leads with data-driven strategies, developing clinical indicators to align care with population needs. She advocates for improved sector-wide data collection to highlight Nurse Practitioner impact. She actively participates in professional organizations such as NPAO and RNAO and serves on planning and advisory committees. Her advocacy for NP-led models contributes to primary care renewal.
As an Adjunct Clinical Professor at Western University, Elizabeth has developed leadership curriculum, mentored students, and participated in graduate panels demonstrating her commitment to preparing future nurse leaders.
Elizabeth leads efforts to expand healthcare team capacity by enabling all professionals to work at their optimal scope. She supports flexible funding models that allow NPs to reach underserved communities.

Jodi Colwill
Driving integrated and equitable primary care
- System-level innovator
- Equity-focused leadership
- Excellent care
As PCN Lead, Jodi coordinates regional team-based care to increase patient attachment. Their leadership drives quality improvement, system integration, and equity-focused strategies.
Jodi fosters collaboration through innovative partnerships and cross-sector initiatives. She has played a key role in the Telepsychiatry Collaborative Care project, a joint effort between AFHTO and NPAO, and has advanced digital solutions in rural primary care settings.
Jodi demonstrates a strong capacity for innovation through her provincial-level advocacy and system planning. She represents Nurse Practitioners in policy discussions and serves as a representative at the Ontario Primary Care Collaborative. As Co-Lead of the Ontario Health Team Community of Practice, she contributes to shaping integrated care models that are responsive to community needs and grounded in evidence-based practice.
Jodi’s tangible impact is most visible in her delivery of high-volume obstetrics care, supporting over 4,000 births annually. Her contributions span triage, labor support, operating room assistance, and postpartum care.

Subo Awan
Transforming teams through equity and quality
- Organizational transformation
- Equity centered leadership
- Quality improvement
Subo revitalized her FHT by formalizing policies, promoting quality improvement, and embedding equity and inclusion. Her leadership has strengthened the team’s ability to serve the community effectively.
Within her organization, she promotes interdisciplinary cooperation and encourages allied health professionals to take on leadership roles and spearhead projects. Externally, she builds bridges with community partners, Indigenous health organizations, and local political representatives.
Subo recognized the need for greater equity and cultural competence and responded by launching educational initiatives that introduced Indigenous health perspectives to her team.
Her leadership has led to improvements in cancer screening rates, patient satisfaction scores, and other clinical performance metrics. Institutionally, she introduced formal staff policies, enhanced the organization’s website, and increased transparency in financial and governance matters. Perhaps most significantly, she has shifted the attitudes of staff, fostering a team that is more positive, quality-focused, and deeply invested in patient outcomes.

Cyril Turley
Pioneering expanded nursing practice
- Collaborative spirit
- Elevating nursing
- First RN prescriber
Cyril was Ontario’s first RN with prescribing authority and has held multiple leadership roles in long-term and community care. His pioneering work continues to elevate nursing practice and consultation.
Cyril is known for his collaborative spirit and ability to inspire others. He works closely with interdisciplinary teams to ensure seamless care delivery and has mentored numerous colleagues in adopting new clinical practices.
As Ontario’s first RN Prescriber, Cyril led the way in implementing prescribing practices within nursing. He developed protocols and training materials to support other nurses in adopting this expanded role. His initiative not only improved patient access to medications but also demonstrated the value of empowering nurses to practice to their full scope.
Cyril’s impact is felt across the community through improved patient outcomes and enhanced team performance. By championing nurse-led initiatives and advocating for system-level change, Cyril has strengthened the capacity of his team and contributed to a more responsive and inclusive healthcare system.

Bathilde Gautier
Strengthening primary care through quality and access
- Quality improvement
- Digital access innovation
- Cross-team collaboration
Bathilde initiated a regional dietitian Community of Practice and a staff-led QI platform, improving care and engagement. She also led advocacy efforts for equitable funding, elevating primary care voices at the policy level.
Bathilde fosters collaboration across six Family Health Teams by aligning Quality Improvement goals and outcomes. She collaborates with system partners like public health units to streamline processes such as vaccine reporting, strengthening intersectoral relationships and improving system responsiveness.
Bathilde led the implementation of online appointment booking for physicians, addressing both administrative burden and patient access. She used this initiative to spark broader conversations about extending digital access to interprofessional providers.
The online booking system has improved patient satisfaction and reduced administrative workload. Her data-driven leadership enhances patient experience, optimizes clinic operations, and supports more responsive, team-based care.

Denis Tsang
Leading digital transformation across the system
- Digital health integration
- Evidence-based improvement
- System-wide impact
Denis has led digital transformation and quality improvement across eight FHTs, enhancing care and operational efficiency. His mentorship and academic contributions have shaped interprofessional collaboration and education in primary care.
Denis has led regional quality improvement initiatives and supported the implementation of digital health solutions that align with provincial standards. Denis’s influence extends to his role as Board Chair of the College of Dietitians of Ontario and as a lecturer at the University of Toronto, where he shapes the next generation of healthcare leaders.
Denis has introduced innovative approaches to digital health integration, including the use of electronic medical records to support equitable patient care. His leadership in quality improvement has resulted in the development of performance measurement frameworks and the implementation of tools that enhance clinical decision-making. Denis’s initiatives are grounded in evidence and tailored to the needs of both patients and providers, demonstrating his ability to translate vision into actionable change.
Denis’s work has had a measurable impact on patient outcomes, team performance, and system-level integration. By embedding digital health strategies into everyday practice, he improved access to care and streamlined workflows across multiple Family Health Teams.

Dr. Shawn Minor
Stabilizing rural primary care systems
- Rural care leadership
- Physician assessment expertise
- Revitalizing primary care
Dr. Minor helped develop and lead PRO, a provincial program assessing internationally trained physicians for rural practice. His local leadership revitalized primary care in Atikokan, securing stable care for 2,800 residents.
Dr. Minor fosters collaboration by training physician colleagues in PRO’s Multiple Mini Interview (MMI) selection process, using his expertise in rural and remote medicine to guide assessments. He is one of the program’s most trusted clinical field assessors, verifying the real-world skills of internationally trained physicians. His mentorship and stewardship of the program have earned him respect across the province, while his influence locally has helped stabilize care delivery in Atikokan.
Dr. Minor led the complete revitalization of primary care in Atikokan, securing stable care for 2,800 residents. His leadership has transformed the community’s access to healthcare, ensuring continuity and quality in a region that previously faced significant challenges.

Chris Cassolato
Building connected and community driven care
Chris has played a key role in shaping the Cambridge and North Dumfries OHT while leading Two Rivers FHT. His inclusive leadership fosters strong staff connections and community engagement.
Chris is known for fostering strong relationships across teams and sectors. He led the Interprofessional Primary Care Team (IPCT) application process, working closely with co-applicant teams to help roster unattached patients to primary care.
One of Chris’s most innovative contributions is leading the first community paramedic program embedded within an Ontario Family Health Team. This initiative strengthens care for patients with complex needs and has been shared through a co-authored research paper to promote system-level learning.
Chris’s leadership has transformed the internal culture of Two Rivers FHT, fostering a positive, inclusive, and mission-driven environment. Through strategic initiatives and compassionate leadership, Chris has improved access to care, enhanced team performance, and contributed meaningfully to the broader healthcare system.

Ale Heddon
Advancing nursing leadership and practice
- Workforce leadership
- Operational excellence
- Practice development
Ale leads over 20 nurses across 18 sites with clear communication, advocacy, and collaborative problem-solving. Her re-election reflects her trusted leadership and commitment to nursing excellence.
Ale fosters collaboration through monthly nursing team meetings focused on quality improvement, workflow optimization, and shared problem-solving. She represents the nursing team at the NYFHT leadership level, ensuring frontline perspectives are included in decision-making.
Ale co-led the RSV Prevention Program, standardizing documentation and data collection for quality improvement. She also developed “The Handguide,” a comprehensive nursing resource presented at AFHTO conferences, and created a preceptor checklist and student placement process to support both current staff and future professionals.
Ale’s leadership has streamlined workflows, improved communication, and fostered interdisciplinary collaboration. She received the inaugural NYFHT Employee of the Year Award, for her contributions to care quality, team cohesion, and system advancement.
THE HEART OF AFHTO TEAMS
Across AFHTO teams, there are many individuals whose presence is essential but often behind the scenes—they embody the spirit of team-based care through compassion, consistency, and quiet leadership. These team members lift others up, help their teams thrive, and contribute to a positive workplace culture. They’re the glue that holds the team together—mentors, supporters, and steady hands who make excellence possible by enabling others to succeed.

Amanda Gallion-Ferron
Delivering compassionate and responsive care
- Trauma-informed care
- Patient-centered
- Supportive team
Amanda fosters a safe, collaborative environment through empathy, openness, and lived experience. Her dedication to team learning and patient comfort strengthens care delivery.
Amanda consistently collaborates with primary care providers to ensure patients receive the most effective treatment possible. She is known for her consistency, dependability, and willingness to support others, which inspires her colleagues and enhances the overall functioning of the team.
Amanda brings creativity and initiative to her role by integrating trauma-informed care and culturally sensitive approaches into her practice. She adapts her methods to meet the unique needs of each patient, often going beyond standard protocols to ensure holistic support.
Amanda’s impact is deeply felt across the Timmins Academic Family Health Team. Her contributions have improved patient outcomes, strengthened interprofessional collaboration, and elevated the standard of care. She is a trusted colleague whose presence enhances team morale and cohesion. Her work not only benefits individual patients but also contributes to a more inclusive and responsive healthcare environment.

Chris LeBouthillier
Thoughtful leadership and mentorship
- Dependable system leader
- Digital health champion
- Inclusive and collaborative
Chris supports nearly every aspect of West Carleton Family Health Team operations with humility and mentorship, enabling others to thrive. His regional leadership in digital health and paramedicine enhances care for vulnerable populations.
As Co-Chair of the Ottawa West Four Rivers Ontario Health Team, he was pivotal in uniting diverse groups into a cohesive application that secured OHT designation in 2021. His ability to bring together health system, primary care, and lived experience partners with compassion and clarity reflects his deep commitment to inclusive leadership.
Chris led the transition to a new electronic medical record system at WCFHT, working nights and weekends to ensure smooth migration with minimal disruption to patient care. He continues to host “lunch and learn” sessions to help staff refine their EMR skills and improve efficiency. Chris’s tireless work ethic and enduring commitment have a profound impact on his team and the broader community.
His mentorship empowers others to lead, and his thoughtful guidance creates space for growth and innovation. Whether through system-level improvements or day-to-day support, Chris embodies the spirit of dependable leadership.

Ellen Ibey
Leading resilient primary care in rural communities
- Empowering team members
- Resilient problem solver
- Trusted mentor
Since 2010, Ellen has grown Temagami Family Health Team (TFHT) from 3 to a full interdisciplinary team, creating a supportive workplace. Her mentorship and adaptability have earned community respect and improved staff development.
Ellen’s mentorship has empowered team members to pursue further education and professional development. She fosters a culture of encouragement and growth, helping staff advance their careers while strengthening the team’s collective capacity.
Whether facing cyber threats, technology malfunctions, or winter highway closures, she treats each obstacle as an opportunity to improve systems and support her team. Her problem-solving and commitment to continuous improvement has helped TFHT navigate complex situations with resilience and grace.
Living and working in a rural, isolated community 60 km from the nearest hospital, Ellen has made it her mission to help people, staff and patients alike. Her compassionate leadership has created a workplace where staff feel valued and supported, and where patients receive care grounded in empathy and excellence. Ellen’s impact is felt not only in the operational success of TFHT but also in the lives she touches every day.

Tara Peel
Expanding access through compassionate leadership
- Clinical leadership
- Program innovator
- Inclusive approach
Tara fosters a collaborative and nurturing environment across all roles from administrative staff to interdisciplinary health professionals and clinicians, and she mentors Registered Nurses and actively supports Nurse Practitioner students from post-graduate institutions.
Her inclusive approach ensures that every team member feels valued and empowered, and her willingness to step in for clinical coverage reinforces her commitment to team continuity and care quality.
Tara’s leadership extends into operational innovation – she contributes to lab management, and group programs for newborns and mothers, prenatal care, and women’s health, including premenopausal and menopausal support. Her continued dedication to the Menopause Clinic has been transformative for patients, offering personalized care and symptom relief that has significantly improved quality of life.
Tara’s impact is felt deeply – she is a wise and compassionate practitioner who listens attentively and provides thoughtful care. She strengthens team cohesion, improves patient outcomes, and expands access to services in Newmarket, Aurora, and Bradford.

Julie MacVoy
Delivering care grounded in trust and empathy
- Holistic care approach
- Strong communicator
- Supportive and professional
Julie fosters collaboration by sharing knowledge generously and advocating fiercely for her patients. Her ability to listen without judgment and communicate complex health issues in a clear, supportive manner inspires confidence and trust among her peers. Testimonials from coworkers highlight her role in strengthening team cohesion and morale, noting that her influence extends beyond clinical care to shaping a culture of mutual respect.
Julie’s approach to care is holistic and proactive. She doesn’t just treat symptoms, she sees the whole person, integrating emotional and psychological support into her clinical practice. Her follow-up is consistent and thoughtful, and she adapts her communication to meet each patient’s needs.
Julie’s impact is felt in both patient outcomes and team dynamics. Patients regularly express how seen and supported they feel under her care, and colleagues describe her as a stabilizing force who brings heart, skill, and professionalism to every interaction. Her contributions have improved the well-being of patients and elevated the standard of care at the clinic. Julie’s legacy is one of kindness, excellence, and enduring influence.

Erika North
Impactful leader supporting growth and comprehensive care
- Quality improvement
- Inclusive care champion
- Clinical innovator
Erika is a grounding presence and a catalyst for growth, offering support that is both gentle and direct when needed. Her leadership in co-creating a comprehensive obesity care pathway including visit templates, patient handouts, and medication charts was a team effort she championed without seeking credit. Her election to the Primary Care Advisory Council further demonstrates the trust and respect she has earned from colleagues.
Erika spearheaded a QI pilot to track physician assistant involvement in obesity management and led the development of practical tools to improve clinician confidence and patient access. Her ability to identify gaps and rally diverse teams to co-create solutions exemplifies her innovative spirit.
Erika’s impact is felt deeply across NYFHT. She creates safe, inclusive spaces where patients and colleagues feel heard and supported. Her compassionate care, especially in mental health, has helped patients navigate anxiety, depression, ADHD, and complex psychosocial stressors. She was honored with NYFHT’s inaugural Excellence in Patient Care Award, a peer-nominated recognition that reflects her profound influence.

Norma Connolly
Strengthening care through education and mentorship
- Interprofessional care champion
- Experienced mentor
- Dynamic and adaptive leadership
Norma teaches across healthcare settings with patience and care, driven by commitment to excellent patient outcomes. Her influence spans nurses, PSWs, and physicians.
Her mentorship helps build confidence and competence among team members, and her ability to connect across disciplines strengthens interprofessional relationships. Norma’s influence is felt not only in clinical outcomes but also in the professional growth of those she supports, making her a trusted and respected figure in her community.
Norma brings innovative approaches to care delivery and staff development, adapting guidance to meet the needs of diverse learners and care environments and ensuring that best practices are shared. Her initiative in creating inclusive learning spaces and promoting continuous improvement elevates the standard of care across the teams she works with.
Nora’s impact is profound and far-reaching. Her dedication has shaped the careers of countless healthcare professionals and she embodies the values of compassion, excellence, and teamwork, making her a true “heart of the team” whose legacy continues to inspire.

Frank Ruberto
A catalyst of team growth
- Equity-focused leadership
- Dedication and commitment
- Culture builder
Frank is a supportive, caring, leader, with a strengths-based and solution-focused approach to any challenge. Frank goes the extra mile in ensuring people feel seen, appreciated, supported and can become a better version of themselves every day. He knows how to bring the best in people and any conversation, especially navigating difficult topics with utmost professionalism.
To him, health equity is something he is able to breathe and demonstrate on a daily basis, and not just something he’s citing in an abstract manner. As a member of an equity deserving group, he brings health equity to the conversation in an intersectional manner, by being respectful, mindful of his own blind spots, asking curious and respectful questions and challenging his own belief.
Frank is an expert at bringing out the best in people and any given situation. He is always finding and proposing new ways for continuous improvement and gets people inspired and motivating by sharing personal learnings and experiences, empowering people to further their learning journeys and being a cohesive, dynamic team. He always offers to support and has a roll-up your sleeves approach, making people confident and energized that they will not feel alone in any endeavour.
AFHTO Teams of the Year
Primary care teams across AFHTO membership exemplify exceptional interprofessional collaboration, patient-centred care, and innovative quality improvement initiatives. These teams are a beacon of inspiration, showcasing remarkable outcomes, fostering an empowering culture, and sharing impactful practices that elevate primary care. Work is always performed by a cohesive team dedicated to transforming care delivery in their professional roles.

Woodbridge Medical Centre Family Health Team
Setting the standard for inclusive and digital primary care
- Shared governance model
- Digital care innovation
- Patient engagement
Woodbridge FHT ensures equal representation across all committees, empowering every discipline to shape care and operations. This inclusive model enhances clinical outcomes, team satisfaction, and quality improvement.
The team exemplifies shared leadership and open communication, with all disciplines contributing to program planning and quality improvement. WMC FHT also engages patients through a Patient Advisory Council, semi-annual experience surveys, and digital tools for booking and messaging.
Recently, the team transitioned from paper-based to digital workflows, integrating AI-powered clinical decision support and virtual tools. Their inclusive structure and digital health initiatives have influenced care models and operational standards across Ontario, serving as a scalable blueprint for other teams.
WMC FHT has achieved measurable improvements in access, efficiency, and satisfaction.
Woodbridge Medical Centre Family Health Team
Setting the standard for inclusive and digital primary care

Norfolk Family Health Team
Delivering coordinated care rooted in community needs
- Co-designed, integrated care
- Interprofessional collaboration
- Community wide access
Norfolk FHT integrates interprofessional collaboration into daily practice, with shared leadership and co-designed programs tailored to rural needs. Their Aging Well and Midwifery programs exemplify holistic, coordinated care.
Interprofessional collaboration is embedded in daily practice. Programs are co-designed using the strengths of each discipline. NFHT also gathers patient input through online surveys, a suggestion box, participation in community events, and targeted focus groups.
NFHT continuously improves programs by incorporating patient feedback and data trends. Since 2018, NFHT has made all programs accessible to the entire Norfolk community, regardless of physician attachment.
NFHT’s integrated care model has led to measurable improvements in access, efficiency, and patient satisfaction. Patients report high satisfaction with timely, comprehensive care.

Barrie and Community Family Health Team
Bringing coordinated care directly to children and families
- Comprehensive pediatric care
- School based delivery
- Family-centered approach
The Barrie and Community FHT supports children with complex needs through coordinated care from nurses, social workers, pediatricians, and therapists. Shared leadership and regular huddles ensure integrated, family-centered support.
Our School Success Program (SSP) exemplifies interprofessional collaboration, with health care providers and school teams working together to deliver holistic care. Regular huddles and shared leadership ensure seamless coordination and responsiveness to student needs. As well, the program is deeply embedded in the community, with strong partnerships across schools and families. Feedback from educators and parents highlight SSP’s role in transforming student outcomes and supporting entire family units holistically.
SSP’s delivery of care within school hours is a key innovation, reducing barriers to access and minimizing disruption to education. This approach is a scalable model for integrated pediatric care that can be replicated regionally and provincially to address service gaps.
The program has measurably improved student success, family well-being, and provider satisfaction.

South East Toronto Family Health Team
Redefining collaborative and equitable primary care
- Collaborative care
- Equity-driven design
- Leader in accreditation
SETFHT dismantles hierarchies to foster inclusive collaboration across clinicians, staff, learners, and community partners.
The team’s exceptional interprofessional collaboration is demonstrated through equal representation of clinical, administrative, and quality improvement staff in decision-making. Regular meetings foster open dialogue, shared leadership, and collective problem-solving. SETFHT also co-designs care with patients and community partners, including a collaborative strategic plan. Ongoing feedback is gathered through advisory committees, forums, and surveys, ensuring culturally safe, equitable care.
SETFHT achieved Accreditation Canada status – the first independent primary care team in Ontario to do so. Their inclusive, collaborative model and integrated pathways have set a provincial precedent, inspiring peer organizations and health networks alike.
SETFHT’s transformation resulted in 35% higher staff engagement, increased patient satisfaction, less fragmented care, better diabetes outcomes, and a 30% drop in mental health wait times.